Diagnosis
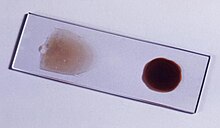
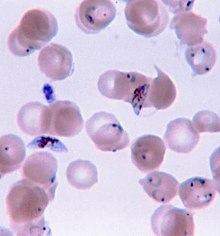
Approximately 30% of people will no longer have a fever upon arriving to a health care facility. Owing to the non-specific nature of the presentation, diagnosis of malaria in non-endemic areas requires a high degree of suspicion, which might be elicited by any of the following: recent travel history, enlarged spleen, fever without localizing signs, low platelets, and hyperbilirubinemia combined with a normal peripheral blood leukocyte count.Malaria is usually confirmed by the microscopic examination of blood films or by antigen-based rapid diagnostic tests (RDT).
Microscopy is the most commonly used method to detect the malarial parasite—about 165 million blood films were examined for malaria in 2010.
Despite its widespread usage, diagnosis by microscopy suffers from two main drawbacks: many settings (especially rural) are not equipped to perform the test, and the accuracy of the results depends on both the skill of the person examining the blood film and the levels of the parasite in the blood.
The sensitivity of blood films ranges from 75–90% in optimum conditions, to as low as 50%. Commercially available RDTs are often more accurate than blood films at predicting the presence of malaria parasites, but they are widely variable in diagnostic sensitivity and specificity depending on manufacturer, and are unable to tell how many parasites are present.
In regions where laboratory tests are readily available, malaria should be suspected, and tested for, in any unwell patient who has been in an area where malaria is endemic.
In areas that cannot afford laboratory diagnostic tests, it has become routine to use only a history of subjective fever as the indication to treat for malaria—a presumptive approach exemplified by the common teaching "fever equals malaria unless proven otherwise".
A drawback of this practice is overdiagnosis of malaria and mismanagement of non-malarial fever, which wastes limited resources, erodes confidence in the health care system, and contributes to drug resistance.
Although polymerase chain reaction-based tests have been developed, these are not widely implemented in malaria-endemic regions as of 2012, due to their complexity.
Classification
Malaria is classified into either "severe" or "uncomplicated" by the World Health Organization (WHO).It is deemed severe when any of the following criteria are present, otherwise it is considered uncomplicated.
- Decreased consciousness
- Significant weakness such that the person is unable to walk
- Inability to feed
- Two or more convulsions
- Low blood pressure (less than 70 mmHg in adults and 50 mmHg in children)
- Breathing problems
- Circulatory shock
- Kidney failure or hemoglobin in the urine
- Bleeding problems, or hemoglobin less than 50 g/L (5 g/dL)
- Pulmonary edema
- Blood glucose less than 2.2 mmol/L (40 mg/dL)
- Acidosis or lactate levels of greater than 5 mmol/L
- A parasite level in the blood of greater than 100,000 per microlitre (µL) in low-intensity transmission areas, or 250,000 per µL in high-intensity transmission areas
Prevention

An Anopheles stephensi
mosquito shortly after obtaining blood from a human (the droplet of
blood is expelled as a surplus).
This mosquito is a vector of malaria, and mosquito control is an effective way of reducing its incidence.
This mosquito is a vector of malaria, and mosquito control is an effective way of reducing its incidence.
If any of these is lowered sufficiently, the parasite will eventually disappear from that area, as happened in North America, Europe and much of the Middle East. However, unless the parasite is eliminated from the whole world, it could become re-established if conditions revert to a combination that favours the parasite's reproduction.
Many researchers argue that prevention of malaria may be more cost-effective than treatment of the disease in the long run, but the capital costs required are out of reach of many of the world's poorest people.
There is a wide disparity in the costs of control (i.e. maintenance of low endemicity) and elimination programs between countries.
For example, in China—whose government in 2010 announced a strategy to pursue malaria elimination in the Chinese provinces—the required investment is a small proportion of public expenditure on health. In contrast, a similar program in Tanzania would cost an estimated one-fifth of the public health budget.
Vector control
Vector control refers to preventative methods used to decrease malaria and morbidity and mortality by reducing the levels of transmission. For individual protection, the most effective chemical insect repellents to reduce human-mosquito contact are those based on DEET and picaridin.Insecticide-treated mosquito nets (ITNs) and indoor residual spraying (IRS) have been shown to be highly effective vector control interventions in preventing malaria morbidity and mortality among children in malaria-endemic settings.
IRS is the practice of spraying insecticides on the interior walls of homes in malaria-affected areas. After feeding, many mosquito species rest on a nearby surface while digesting the bloodmeal, so if the walls of dwellings have been coated with insecticides, the resting mosquitoes can be killed before they can bite another victim and transfer the malaria parasite.
As of 2006, the World Health Organization advises the use of 12 insecticides in IRS operations, including DDT and the pyrethroids cyfluthrin and deltamethrin.
This public health use of small amounts of DDT is permitted under the Stockholm Convention on Persistent Organic Pollutants (POPs), which prohibits the agricultural use of DDT.
One problem with all forms of IRS is insecticide resistance via evolution. Mosquitoes affected by IRS tend to rest and live indoors, and due to the irritation caused by spraying, their descendants tend to rest and live outdoors, meaning that they are less affected by the IRS, which greatly reduces its effectiveness as a defense mechanism.
Mosquito nets help keep mosquitoes away from people and significantly reduce infection rates and transmission of malaria.
Nets are not a perfect barrier and are often treated with an insecticide designed to kill the mosquito before it has time to find a way past the net.
Insecticide-treated nets are estimated to be twice as effective as untreated nets and offer greater than 70% protection compared with no net.
Between 2000 and 2008, the use of ITNs saved the lives of an estimated 250,000 infants in Sub-Saharan Africa.
Although ITNs prevent malaria, only about 13% of households in Sub-Saharan countries own them.
A recommended practice for usage is to hang a large "bed net" above the center of a bed to drape over it completely with the edges tucked in. Pyrethroid-treated nets and long-lasting insecticide-treated nets offer the best personal protection, and are most effective when used from dusk to dawn.
Other methods
Community participation and health education strategies promoting awareness of malaria and the importance of control measures have been successfully used to reduce the incidence of malaria in some areas of the developing world.Recognizing the disease in the early stages can stop the disease from becoming fatal. Education can also inform people to cover over areas of stagnant, still water, such as water tanks that are ideal breeding grounds for the parasite and mosquito, thus cutting down the risk of the transmission between people.
This is generally used in urban areas where there are large centers of population in a confined space and transmission would be most likely in these areas.
Intermittent preventive therapy is another intervention that has been used successfully to control malaria in pregnant women and infants, and in preschool children where transmission is seasonal.
Medications
Several drugs, most of which are used for treatment of malaria, can be taken to prevent contracting the disease during travel to endemic areas. Chloroquine may be used where the parasite is still sensitive.Because of the prevalence of drug-resistant Plasmodium, one of three medications—mefloquine (Lariam), doxycycline (available generically), or the combination of atovaquone and proguanil hydrochloride (Malarone)—is frequently needed.
Doxycycline and the atovaquone and proguanil combination are the best tolerated; mefloquine is associated with death, suicide, and higher rates of neurological and psychiatric symptoms.
The prophylactic effect does not begin immediately upon starting the drugs, so people temporarily visiting malaria-endemic areas usually begin taking the drugs one to two weeks before arriving and should continue taking them for four weeks after leaving (with the exception of atovaquone proguanil that only needs to be started two days prior and continued for seven days afterwards).
Use of prophylactic drugs is seldom practical for full-time residents of malaria-endemic areas, and their use is usually restricted to short-term visitors and travellers to malarial regions.
This is due to the cost of purchasing the drugs, negative adverse effects from long-term use, and because some effective anti-malarial drugs are difficult to obtain outside of wealthy nations.
The use of prophylactic drugs where malaria-bearing mosquitoes are present may encourage the development of partial immunity.
Treatment
The treatment of malaria depends on the severity of the disease. Uncomplicated malaria may be treated with oral medications. The most effective strategy for P. falciparum infection is the use of artemisinins in combination with other antimalarials (known as artemisinin-combination therapy, or ACT), which reduces the ability of the parasite to develop resistance to any single drug component.These additional antimalarials include amodiaquine, lumefantrine, mefloquine or sulfadoxine/pyrimethamine.
Another recommended combination is dihydroartemisinin and piperaquine. ACT is about 90% effective when used to treat uncomplicated malaria.
To treat malaria during pregnancy, the WHO recommends the use of quinine plus clindamycin early in the pregnancy (1st trimester), and ACT in later stages (2nd and 3rd trimesters).
In the 2000s (decade), malaria with partial resistance to artemisins emerged in Southeast Asia.
Severe malaria requires the parenteral administration of antimalarial drugs. Until the mid-2000s the most used treatment for severe malaria was quinine, but artesunate has been shown to be superior to quinine in both children and adults.
Treatment of severe malaria also involves supportive measures that are optimally performed in a critical care unit, including management of high fevers (hyperpyrexia) and the subsequent seizures that may result from it, and monitoring for respiratory depression, hypoglycemia, and hypokalemia.
Infection with P. vivax, P. ovale or P. malariae is usually treated on an outpatient basis (while a person is at home). Treatment of P. vivax requires both treatment of blood stages (with chloroquine or ACT) as well as clearance of liver forms with primaquine.
















The liver could be a vitals gift in vertebrates and a few different animals. it's a large vary of functions, together with detoxification, supermolecule synthesis, and production of biochemicals necessary for digestion. The symptoms associated with liver disfunction embrace each physical signs and a spread of symptoms associated with organic process issues, blood glucose issues, immune disorders, abnormal absorption of fats, and metabolism issues.
ReplyDelete