Alzheimer's disease (AD), also known in medical literature as Alzheimer disease, is the most common form of dementia.
There is no cure for the disease, which worsens as it progresses, and eventually leads to death. It was first described by German psychiatrist and neuropathologist Alois Alzheimer in 1906 and was named after him.[1]
Most often, AD is diagnosed in people over 65 years of age,[2] although the less-prevalent early-onset Alzheimer's can occur much earlier. In 2006, there were 26.6 million sufferers worldwide. Alzheimer's is predicted to affect 1 in 85 people globally by 2050.[3]
Although Alzheimer's disease develops differently for every individual, there are many common symptoms.[4]
Early symptoms are often mistakenly thought to be 'age-related' concerns, or manifestations of stress.[5]
In the early stages, the most common symptom is difficulty in remembering recent events.
When AD is suspected, the diagnosis is usually confirmed with tests that evaluate behaviour and thinking abilities, often followed by a brain scan if available.[6]
As the disease advances, symptoms can include confusion, irritability, aggression, mood swings, trouble with language, and long-term memory loss.
As the sufferer declines they often withdraw from family and society.[5][7] Gradually, bodily functions are lost, ultimately leading to death.[8]
Since the disease is different for each individual, predicting how it will affect the person is difficult. AD develops for an unknown and variable amount of time before becoming fully apparent, and it can progress undiagnosed for years.
On average, the life expectancy following diagnosis is approximately seven years.[9] Fewer than three percent of individuals live more than fourteen years after diagnosis.[10]
The cause and progression of Alzheimer's disease are not well understood. Research indicates that the disease is associated with plaques and tangles in the brain.[11]
Current treatments only help with the symptoms of the disease. There are no available treatments that stop or reverse the progression of the disease. As of 2012, more than 1,000 clinical trials have been or are being conducted to test various compounds in AD.[12]
Mental stimulation, exercise, and a balanced diet have been suggested as ways to delay cognitive symptoms (though not brain pathology) in healthy older individuals, but there is no conclusive evidence supporting an effect.[13]
Because AD cannot be cured and is degenerative, the sufferer relies on others for assistance. The role of the main caregiver is often taken by the spouse or a close relative.[14]
Alzheimer's disease is known for placing a great burden on caregivers; the pressures can be wide-ranging, involving social, psychological, physical, and economic elements of the caregiver's life.[15][16][17] In developed countries, AD is one of the most costly diseases to society.
The cholinergic hypothesis has not maintained widespread support, largely because medications intended to treat acetylcholine deficiency have not been very effective. Other cholinergic effects have also been proposed, for example, initiation of large-scale aggregation of amyloid,[36] leading to generalised neuroinflammation.[37]
Also, a specific isoform of apolipoprotein, APOE4, is a major genetic risk factor for AD. Whilst apolipoproteins enhance the breakdown of beta amyloid, some isoforms are not very effective at this task (such as APOE4), leading to excess amyloid buildup in the brain.[42]
Further evidence comes from the finding that transgenic mice that express a mutant form of the human APP gene develop fibrillar amyloid plaques and Alzheimer's-like brain pathology with spatial learning deficits.[43]
An experimental vaccine was found to clear the amyloid plaques in early human trials, but it did not have any significant effect on dementia.[44]
Researchers have been led to suspect non-plaque Aβ oligomers (aggregates of many monomers) as the primary pathogenic form of Aβ.
These toxic oligomers, also referred to as amyloid-derived diffusible ligands (ADDLs), bind to a surface receptor on neurons and change the structure of the synapse, thereby disrupting neuronal communication.[45]
One receptor for Aβ oligomers may be the prion protein, the same protein that has been linked to mad cow disease and the related human condition, Creutzfeldt–Jakob disease, thus potentially linking the underlying mechanism of these neurodegenerative disorders with that of Alzheimer's disease.[46]
In 2009, this theory was updated, suggesting that a close relative of the beta-amyloid protein, and not necessarily the beta-amyloid itself, may be a major culprit in the disease.
The theory holds that an amyloid-related mechanism that prunes neuronal connections in the brain in the fast-growth phase of early life may be triggered by ageing-related processes in later life to cause the neuronal withering of Alzheimer's disease.[47]
N-APP, a fragment of APP from the peptide's N-terminus, is adjacent to beta-amyloid and is cleaved from APP by one of the same enzymes.
N-APP triggers the self-destruct pathway by binding to a neuronal receptor called death receptor 6 (DR6, also known as TNFRSF21).[47] DR6 is highly expressed in the human brain regions most affected by Alzheimer's, so it is possible that the N-APP/DR6 pathway might be hijacked in the ageing brain to cause damage. In this model, beta-amyloid plays a complementary role, by depressing synaptic function.
Eventually, they form neurofibrillary tangles inside nerve cell bodies.[48] When this occurs, the microtubules disintegrate, collapsing the neuron's transport system.[49] This may result first in malfunctions in biochemical communication between neurons and later in the death of the cells.[50]
Another hypothesis asserts that the disease may be caused by age-related myelin breakdown in the brain. Iron released during myelin breakdown is hypothesised to cause further damage. Homeostatic myelin repair processes contribute to the development of proteinaceous deposits such as beta-amyloid and tau.[52][53][54]
Oxidative stress and dys-homeostasis of biometal (biology) metabolism may be significant in the formation of the pathology.[55][56]
AD individuals show 70% loss of locus coeruleus cells that provide norepinephrine (in addition to its neurotransmitter role) that locally diffuses from "varicosities" as an endogenous anti-inflammatory agent in the microenvironment around the neurons, glial cells, and blood vessels in the neocortex and hippocampus.[57]
It has been shown that norepinephrine stimulates mouse microglia to suppress Aβ-induced production of cytokines and their phagocytosis of Aβ.[57] This suggests that degeneration of the locus ceruleus might be responsible for increased Aβ deposition in AD brains.
Accumulation of aggregated amyloid fibrils, which are believed to be the toxic form of the protein responsible for disrupting the cell's calcium ion homeostasis, induces programmed cell death (apoptosis).[71]
It is also known that Aβ selectively builds up in the mitochondria in the cells of Alzheimer's-affected brains, and it also inhibits certain enzyme functions and the utilisation of glucose by neurons.[72]
Various inflammatory processes and cytokines may also have a role in the pathology of Alzheimer's disease. Inflammation is a general marker of tissue damage in any disease, and may be either secondary to tissue damage in AD or a marker of an immunological response.[73]
Alterations in the distribution of different neurotrophic factors and in the expression of their receptors such as the brain-derived neurotrophic factor (BDNF) have been described in AD.[74][75]
This form of the disease is known as early onset familial Alzheimer's disease.
Most of autosomal dominant familial AD can be attributed to mutations in one of three genes: amyloid precursor protein (APP) and presenilins 1 and 2.[77]
Most mutations in the APP and presenilin genes increase the production of a small protein called Aβ42, which is the main component of senile plaques.[78] Some of the mutations merely alter the ratio between Aβ42 and the other major forms—e.g., Aβ40—without increasing Aβ42 levels.[78][79]
This suggests that presenilin mutations can cause disease even if they lower the total amount of Aβ produced and may point to other roles of presenilin or a role for alterations in the function of APP and/or its fragments other than Aβ.
Most cases of Alzheimer's disease do not exhibit autosomal-dominant inheritance and are termed sporadic AD. Nevertheless genetic differences may act as risk factors. The best known genetic risk factor is the inheritance of the ε4 allele of the apolipoprotein E (APOE).[80][81]
Between 40 and 80% of people with AD possess at least one APOEε4 allele.[81] The APOEε4 allele increases the risk of the disease by three times in heterozygotes and by 15 times in homozygotes.[76] However, this "genetic" effect is not necessarily purely genetic. For example, certain Nigerian populations have no relationship between presence or dose of APOEε4 and incidence or age-of-onset for Alzheimer's disease.[82][83]
Geneticists agree that numerous other genes also act as risk factors or have protective effects that influence the development of late onset Alzheimer's disease,[77] but results such as the Nigerian studies and the incomplete penetrance for all genetic risk factors associated with sporadic Alzheimers indicate a strong role for environmental effects. Over 400 genes have been tested for association with late-onset sporadic AD,[77] most with null results.[76]
Mutations in the TREM2 gene have been associated with a 3 to 5 times higher risk of developing Alzheimer's disease.[84][85] A suggested mechanism of action is that when TREM2 is mutated, white blood cells in the brain are no longer able to control the amount of beta amyloid present.
Moreover, it may predict conversion from prodromal stages (mild cognitive impairment) to Alzheimer's disease.[89]
Assessment of intellectual functioning including memory testing can further characterise the state of the disease.[5]
Medical organisations have created diagnostic criteria to ease and standardise the diagnostic process for practicing physicians. The diagnosis can be confirmed with very high accuracy post-mortem when brain material is available and can be examined histologically.[90]
Neuropsychological tests such as the mini–mental state examination
(MMSE) are widely used to evaluate the cognitive impairments needed for
diagnosis.
More comprehensive test arrays are necessary for high reliability of results, particularly in the earliest stages of the disease.[95][96] Neurological examination in early AD will usually provide normal results, except for obvious cognitive impairment, which may not differ from that resulting from other diseases processes, including other causes of dementia.
Further neurological examinations are crucial in the differential diagnosis of AD and other diseases.[5] Interviews with family members are also utilised in the assessment of the disease. Caregivers can supply important information on the daily living abilities, as well as on the decrease, over time, of the person's mental function.[89]
A caregiver's viewpoint is particularly important, since a person with AD is commonly unaware of his own deficits.[97] Many times, families also have difficulties in the detection of initial dementia symptoms and may not communicate accurate information to a physician.[98]
Another recent objective marker of the disease is the analysis of cerebrospinal fluid for beta-amyloid or tau proteins,[99] both total tau protein and phosphorylated tau181P protein concentrations.[100]
Searching for these proteins using a spinal tap can predict the onset of Alzheimer's with a sensitivity of between 94% and 100%.[100]
When used in conjunction with existing neuroimaging techniques, doctors can identify people with significant memory loss who are already developing the disease.[100] Spinal fluid tests are commercially available, unlike the latest neuroimaging technology.[101]
Alzheimer's was diagnosed in one-third of the people who did not have any symptoms in a 2010 study, meaning that disease progression occurs well before symptoms occur.[102]
Supplemental testing provides extra information on some features of the disease or is used to rule out other diagnoses. Blood tests can identify other causes for dementia than AD[5]—causes which may, in rare cases, be reversible.[103]
It is common to perform thyroid function tests, assess B12, rule out syphilis, rule out metabolic problems (including tests for kidney function, electrolyte levels and for diabetes), assess levels of heavy metals (e.g. lead, mercury) and anaemia. (See differential diagnosis for Dementia). (It is also necessary to rule out delirium).
Psychological tests for depression are employed, since depression can either be concurrent with AD (see Depression of Alzheimer disease), an early sign of cognitive impairment,[104] or even the cause.[105][106]
However, epidemiological studies have proposed relationships between certain modifiable factors, such as diet, cardiovascular risk, pharmaceutical products, or intellectual activities among others, and a population's likelihood of developing AD.
Only further research, including clinical trials, will reveal whether these factors can help to prevent AD.[108]
Although cardiovascular risk factors, such as hypercholesterolaemia, hypertension, diabetes, and smoking, are associated with a higher risk of onset and course of AD,[109][110] statins, which are cholesterol lowering drugs, have not been effective in preventing or improving the course of the disease.[111][112]
The components of a Mediterranean diet, which include fruit and vegetables, bread, wheat and other cereals, olive oil, fish, and red wine, may all individually or together reduce the risk and course of Alzheimer's disease.[113] The diet's beneficial cardiovascular effect has been proposed as the mechanism of action.[113]
There is limited evidence that light to moderate use of alcohol, particularly red wine, is associated with lower risk of AD.[114]
Reviews on the use of vitamins have not found enough evidence of efficacy to recommend vitamin C,[115] E,[115][116] or folic acid with or without vitamin B12,[117] as preventive or treatment agents in AD. Additionally vitamin E is associated with health risks.[115]
Trials examining folic acid (B9) and other B vitamins failed to show any significant association with cognitive decline.[118] Docosahexaenoic acid, an Omega 3 fatty acid, has not been found to slow decline.[119]
Long-term usage of non-steroidal anti-inflammatory drug (NSAIDs) is associated with a reduced likelihood of developing AD.[120]
Human postmortem studies, in animal models, or in vitro investigations also support the notion that NSAIDs can reduce inflammation related to amyloid plaques.[120] However trials investigating their use as palliative treatment have failed to show positive results while no prevention trial has been completed.[120]
Hormone replacement therapy, although previously used, may increase the risk of dementia.[121]
Curcumin as of 2010 has not shown benefit in people even though there is tentative evidence in animals.[122] There is inconsistent and unconvincing evidence that ginkgo has any positive effect on cognitive impairment and dementia,[123] and a recent study concludes that it has no effect in reducing the rate of AD incidence.[124]
There is tentative evidence that caffeine may be protective.[125] As of 2008 there is no concrete evidence that cannabinoids are effective in improving the symptoms of AD or dementia.[126] Some research in its early stages however looks promising.[127]
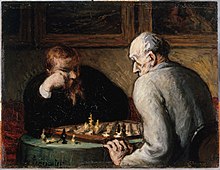
People who engage in intellectual activities such as reading, playing board games, completing crossword puzzles, playing musical instruments, or regular social interaction show a reduced risk for Alzheimer's disease.[128]
This is compatible with the cognitive reserve theory, which states that some life experiences result in more efficient neural functioning providing the individual a cognitive reserve that delays the onset of dementia manifestations.[128] Education delays the onset of AD syndrome, but is not related to earlier death after diagnosis.[129]
Learning a second language even later in life seems to delay getting Alzheimer disease.[130] Physical activity is also associated with a reduced risk of AD.[129]
Some studies have shown an increased risk of developing AD with environmental factors such the intake of metals, particularly aluminium.[131] The quality of some of these studies has been criticised,[132] and other studies have concluded that there is no relationship between these environmental factors and the development of AD.[133]
While some studies suggest that extremely low frequency electromagnetic fields may increase the risk for Alzheimer's disease,[citation needed] reviewers found that further epidemiological and laboratory investigations of this hypothesis are needed.[134] Smoking is a significant AD risk factor.[135] Systemic markers of the innate immune system are risk factors for late-onset AD
There is no cure for the disease, which worsens as it progresses, and eventually leads to death. It was first described by German psychiatrist and neuropathologist Alois Alzheimer in 1906 and was named after him.[1]
Most often, AD is diagnosed in people over 65 years of age,[2] although the less-prevalent early-onset Alzheimer's can occur much earlier. In 2006, there were 26.6 million sufferers worldwide. Alzheimer's is predicted to affect 1 in 85 people globally by 2050.[3]
Although Alzheimer's disease develops differently for every individual, there are many common symptoms.[4]
Early symptoms are often mistakenly thought to be 'age-related' concerns, or manifestations of stress.[5]
In the early stages, the most common symptom is difficulty in remembering recent events.
When AD is suspected, the diagnosis is usually confirmed with tests that evaluate behaviour and thinking abilities, often followed by a brain scan if available.[6]
As the disease advances, symptoms can include confusion, irritability, aggression, mood swings, trouble with language, and long-term memory loss.
As the sufferer declines they often withdraw from family and society.[5][7] Gradually, bodily functions are lost, ultimately leading to death.[8]
Since the disease is different for each individual, predicting how it will affect the person is difficult. AD develops for an unknown and variable amount of time before becoming fully apparent, and it can progress undiagnosed for years.
On average, the life expectancy following diagnosis is approximately seven years.[9] Fewer than three percent of individuals live more than fourteen years after diagnosis.[10]
The cause and progression of Alzheimer's disease are not well understood. Research indicates that the disease is associated with plaques and tangles in the brain.[11]
Current treatments only help with the symptoms of the disease. There are no available treatments that stop or reverse the progression of the disease. As of 2012, more than 1,000 clinical trials have been or are being conducted to test various compounds in AD.[12]
Mental stimulation, exercise, and a balanced diet have been suggested as ways to delay cognitive symptoms (though not brain pathology) in healthy older individuals, but there is no conclusive evidence supporting an effect.[13]
Because AD cannot be cured and is degenerative, the sufferer relies on others for assistance. The role of the main caregiver is often taken by the spouse or a close relative.[14]
Alzheimer's disease is known for placing a great burden on caregivers; the pressures can be wide-ranging, involving social, psychological, physical, and economic elements of the caregiver's life.[15][16][17] In developed countries, AD is one of the most costly diseases to society.
Cause
The cause for most Alzheimer's cases is still essentially unknown[34] (except for 1% to 5% of cases where genetic differences have been identified). Several competing hypotheses exist trying to explain the cause of the disease:
Cholinergic hypothesis
The oldest, on which most currently available drug therapies are based, is the cholinergic hypothesis,[35] which proposes that AD is caused by reduced synthesis of the neurotransmitter acetylcholine.The cholinergic hypothesis has not maintained widespread support, largely because medications intended to treat acetylcholine deficiency have not been very effective. Other cholinergic effects have also been proposed, for example, initiation of large-scale aggregation of amyloid,[36] leading to generalised neuroinflammation.[37]
Amyloid hypothesis
In 1991, the amyloid hypothesis postulated that beta-amyloid (Aβ) deposits are the fundamental cause of the disease.[38][39] Support for this postulate comes from the location of the gene for the amyloid precursor protein (APP) on chromosome 21, together with the fact that people with trisomy 21 (Down Syndrome) who have an extra gene copy almost universally exhibit AD by 40 years of age.[40][41]Also, a specific isoform of apolipoprotein, APOE4, is a major genetic risk factor for AD. Whilst apolipoproteins enhance the breakdown of beta amyloid, some isoforms are not very effective at this task (such as APOE4), leading to excess amyloid buildup in the brain.[42]
Further evidence comes from the finding that transgenic mice that express a mutant form of the human APP gene develop fibrillar amyloid plaques and Alzheimer's-like brain pathology with spatial learning deficits.[43]
An experimental vaccine was found to clear the amyloid plaques in early human trials, but it did not have any significant effect on dementia.[44]
Researchers have been led to suspect non-plaque Aβ oligomers (aggregates of many monomers) as the primary pathogenic form of Aβ.
These toxic oligomers, also referred to as amyloid-derived diffusible ligands (ADDLs), bind to a surface receptor on neurons and change the structure of the synapse, thereby disrupting neuronal communication.[45]
One receptor for Aβ oligomers may be the prion protein, the same protein that has been linked to mad cow disease and the related human condition, Creutzfeldt–Jakob disease, thus potentially linking the underlying mechanism of these neurodegenerative disorders with that of Alzheimer's disease.[46]
In 2009, this theory was updated, suggesting that a close relative of the beta-amyloid protein, and not necessarily the beta-amyloid itself, may be a major culprit in the disease.
The theory holds that an amyloid-related mechanism that prunes neuronal connections in the brain in the fast-growth phase of early life may be triggered by ageing-related processes in later life to cause the neuronal withering of Alzheimer's disease.[47]
N-APP, a fragment of APP from the peptide's N-terminus, is adjacent to beta-amyloid and is cleaved from APP by one of the same enzymes.
N-APP triggers the self-destruct pathway by binding to a neuronal receptor called death receptor 6 (DR6, also known as TNFRSF21).[47] DR6 is highly expressed in the human brain regions most affected by Alzheimer's, so it is possible that the N-APP/DR6 pathway might be hijacked in the ageing brain to cause damage. In this model, beta-amyloid plays a complementary role, by depressing synaptic function.
Tau hypothesis
The tau hypothesis is the idea that tau protein abnormalities initiate the disease cascade.[39] In this model, hyperphosphorylated tau begins to pair with other threads of tau.Eventually, they form neurofibrillary tangles inside nerve cell bodies.[48] When this occurs, the microtubules disintegrate, collapsing the neuron's transport system.[49] This may result first in malfunctions in biochemical communication between neurons and later in the death of the cells.[50]
Other hypotheses
Herpes simplex virus type 1 has also been proposed to play a causative role in people carrying the susceptible versions of the apoE gene.[51]Another hypothesis asserts that the disease may be caused by age-related myelin breakdown in the brain. Iron released during myelin breakdown is hypothesised to cause further damage. Homeostatic myelin repair processes contribute to the development of proteinaceous deposits such as beta-amyloid and tau.[52][53][54]
Oxidative stress and dys-homeostasis of biometal (biology) metabolism may be significant in the formation of the pathology.[55][56]
AD individuals show 70% loss of locus coeruleus cells that provide norepinephrine (in addition to its neurotransmitter role) that locally diffuses from "varicosities" as an endogenous anti-inflammatory agent in the microenvironment around the neurons, glial cells, and blood vessels in the neocortex and hippocampus.[57]
It has been shown that norepinephrine stimulates mouse microglia to suppress Aβ-induced production of cytokines and their phagocytosis of Aβ.[57] This suggests that degeneration of the locus ceruleus might be responsible for increased Aβ deposition in AD brains.
Disease mechanism
Exactly how disturbances of production and aggregation of the beta-amyloid peptide gives rise to the pathology of AD is not known.[69][70] The amyloid hypothesis traditionally points to the accumulation of beta-amyloid peptides as the central event triggering neuron degeneration.Accumulation of aggregated amyloid fibrils, which are believed to be the toxic form of the protein responsible for disrupting the cell's calcium ion homeostasis, induces programmed cell death (apoptosis).[71]
It is also known that Aβ selectively builds up in the mitochondria in the cells of Alzheimer's-affected brains, and it also inhibits certain enzyme functions and the utilisation of glucose by neurons.[72]
Various inflammatory processes and cytokines may also have a role in the pathology of Alzheimer's disease. Inflammation is a general marker of tissue damage in any disease, and may be either secondary to tissue damage in AD or a marker of an immunological response.[73]
Alterations in the distribution of different neurotrophic factors and in the expression of their receptors such as the brain-derived neurotrophic factor (BDNF) have been described in AD.[74][75]
Genetics
The vast majority of cases of Alzheimer's disease are sporadic, meaning that they are not genetically inherited although some genes may act as risk factors. On the other hand, around 0.1% of the cases are familial forms of autosomal dominant (not sex-linked) inheritance, which usually have an onset before age 65.[76]This form of the disease is known as early onset familial Alzheimer's disease.
Most of autosomal dominant familial AD can be attributed to mutations in one of three genes: amyloid precursor protein (APP) and presenilins 1 and 2.[77]
Most mutations in the APP and presenilin genes increase the production of a small protein called Aβ42, which is the main component of senile plaques.[78] Some of the mutations merely alter the ratio between Aβ42 and the other major forms—e.g., Aβ40—without increasing Aβ42 levels.[78][79]
This suggests that presenilin mutations can cause disease even if they lower the total amount of Aβ produced and may point to other roles of presenilin or a role for alterations in the function of APP and/or its fragments other than Aβ.
Most cases of Alzheimer's disease do not exhibit autosomal-dominant inheritance and are termed sporadic AD. Nevertheless genetic differences may act as risk factors. The best known genetic risk factor is the inheritance of the ε4 allele of the apolipoprotein E (APOE).[80][81]
Between 40 and 80% of people with AD possess at least one APOEε4 allele.[81] The APOEε4 allele increases the risk of the disease by three times in heterozygotes and by 15 times in homozygotes.[76] However, this "genetic" effect is not necessarily purely genetic. For example, certain Nigerian populations have no relationship between presence or dose of APOEε4 and incidence or age-of-onset for Alzheimer's disease.[82][83]
Geneticists agree that numerous other genes also act as risk factors or have protective effects that influence the development of late onset Alzheimer's disease,[77] but results such as the Nigerian studies and the incomplete penetrance for all genetic risk factors associated with sporadic Alzheimers indicate a strong role for environmental effects. Over 400 genes have been tested for association with late-onset sporadic AD,[77] most with null results.[76]
Mutations in the TREM2 gene have been associated with a 3 to 5 times higher risk of developing Alzheimer's disease.[84][85] A suggested mechanism of action is that when TREM2 is mutated, white blood cells in the brain are no longer able to control the amount of beta amyloid present.
Diagnosis
Alzheimer's disease is usually diagnosed clinically from the patient history, collateral history from relatives, and clinical observations, based on the presence of characteristic neurological and neuropsychological features and the absence of alternative conditions.[86][87] Advanced medical imaging with computed tomography (CT) or magnetic resonance imaging (MRI), and with single-photon emission computed tomography (SPECT) or positron emission tomography (PET) can be used to help exclude other cerebral pathology or subtypes of dementia.[88]Moreover, it may predict conversion from prodromal stages (mild cognitive impairment) to Alzheimer's disease.[89]
Assessment of intellectual functioning including memory testing can further characterise the state of the disease.[5]
Medical organisations have created diagnostic criteria to ease and standardise the diagnostic process for practicing physicians. The diagnosis can be confirmed with very high accuracy post-mortem when brain material is available and can be examined histologically.[90]
Technique
More comprehensive test arrays are necessary for high reliability of results, particularly in the earliest stages of the disease.[95][96] Neurological examination in early AD will usually provide normal results, except for obvious cognitive impairment, which may not differ from that resulting from other diseases processes, including other causes of dementia.
Further neurological examinations are crucial in the differential diagnosis of AD and other diseases.[5] Interviews with family members are also utilised in the assessment of the disease. Caregivers can supply important information on the daily living abilities, as well as on the decrease, over time, of the person's mental function.[89]
A caregiver's viewpoint is particularly important, since a person with AD is commonly unaware of his own deficits.[97] Many times, families also have difficulties in the detection of initial dementia symptoms and may not communicate accurate information to a physician.[98]
Another recent objective marker of the disease is the analysis of cerebrospinal fluid for beta-amyloid or tau proteins,[99] both total tau protein and phosphorylated tau181P protein concentrations.[100]
Searching for these proteins using a spinal tap can predict the onset of Alzheimer's with a sensitivity of between 94% and 100%.[100]
When used in conjunction with existing neuroimaging techniques, doctors can identify people with significant memory loss who are already developing the disease.[100] Spinal fluid tests are commercially available, unlike the latest neuroimaging technology.[101]
Alzheimer's was diagnosed in one-third of the people who did not have any symptoms in a 2010 study, meaning that disease progression occurs well before symptoms occur.[102]
Supplemental testing provides extra information on some features of the disease or is used to rule out other diagnoses. Blood tests can identify other causes for dementia than AD[5]—causes which may, in rare cases, be reversible.[103]
It is common to perform thyroid function tests, assess B12, rule out syphilis, rule out metabolic problems (including tests for kidney function, electrolyte levels and for diabetes), assess levels of heavy metals (e.g. lead, mercury) and anaemia. (See differential diagnosis for Dementia). (It is also necessary to rule out delirium).
Psychological tests for depression are employed, since depression can either be concurrent with AD (see Depression of Alzheimer disease), an early sign of cognitive impairment,[104] or even the cause.[105][106]
Prevention
At present, there is no definitive evidence to support that any particular measure is effective in preventing AD.[107] Global studies of measures to prevent or delay the onset of AD have often produced inconsistent results.However, epidemiological studies have proposed relationships between certain modifiable factors, such as diet, cardiovascular risk, pharmaceutical products, or intellectual activities among others, and a population's likelihood of developing AD.
Only further research, including clinical trials, will reveal whether these factors can help to prevent AD.[108]
Although cardiovascular risk factors, such as hypercholesterolaemia, hypertension, diabetes, and smoking, are associated with a higher risk of onset and course of AD,[109][110] statins, which are cholesterol lowering drugs, have not been effective in preventing or improving the course of the disease.[111][112]
The components of a Mediterranean diet, which include fruit and vegetables, bread, wheat and other cereals, olive oil, fish, and red wine, may all individually or together reduce the risk and course of Alzheimer's disease.[113] The diet's beneficial cardiovascular effect has been proposed as the mechanism of action.[113]
There is limited evidence that light to moderate use of alcohol, particularly red wine, is associated with lower risk of AD.[114]
Reviews on the use of vitamins have not found enough evidence of efficacy to recommend vitamin C,[115] E,[115][116] or folic acid with or without vitamin B12,[117] as preventive or treatment agents in AD. Additionally vitamin E is associated with health risks.[115]
Trials examining folic acid (B9) and other B vitamins failed to show any significant association with cognitive decline.[118] Docosahexaenoic acid, an Omega 3 fatty acid, has not been found to slow decline.[119]
Long-term usage of non-steroidal anti-inflammatory drug (NSAIDs) is associated with a reduced likelihood of developing AD.[120]
Human postmortem studies, in animal models, or in vitro investigations also support the notion that NSAIDs can reduce inflammation related to amyloid plaques.[120] However trials investigating their use as palliative treatment have failed to show positive results while no prevention trial has been completed.[120]
Hormone replacement therapy, although previously used, may increase the risk of dementia.[121]
Curcumin as of 2010 has not shown benefit in people even though there is tentative evidence in animals.[122] There is inconsistent and unconvincing evidence that ginkgo has any positive effect on cognitive impairment and dementia,[123] and a recent study concludes that it has no effect in reducing the rate of AD incidence.[124]
There is tentative evidence that caffeine may be protective.[125] As of 2008 there is no concrete evidence that cannabinoids are effective in improving the symptoms of AD or dementia.[126] Some research in its early stages however looks promising.[127]
People who engage in intellectual activities such as reading, playing board games, completing crossword puzzles, playing musical instruments, or regular social interaction show a reduced risk for Alzheimer's disease.[128]
This is compatible with the cognitive reserve theory, which states that some life experiences result in more efficient neural functioning providing the individual a cognitive reserve that delays the onset of dementia manifestations.[128] Education delays the onset of AD syndrome, but is not related to earlier death after diagnosis.[129]
Learning a second language even later in life seems to delay getting Alzheimer disease.[130] Physical activity is also associated with a reduced risk of AD.[129]
Some studies have shown an increased risk of developing AD with environmental factors such the intake of metals, particularly aluminium.[131] The quality of some of these studies has been criticised,[132] and other studies have concluded that there is no relationship between these environmental factors and the development of AD.[133]
While some studies suggest that extremely low frequency electromagnetic fields may increase the risk for Alzheimer's disease,[citation needed] reviewers found that further epidemiological and laboratory investigations of this hypothesis are needed.[134] Smoking is a significant AD risk factor.[135] Systemic markers of the innate immune system are risk factors for late-onset AD














0 comments:
Post a Comment