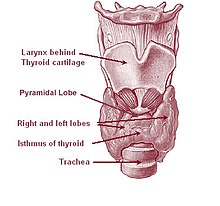
The thyroid gland or simply, the thyroid, in vertebrate anatomy, is one of the largest endocrine glands and consists of two connected lobes. The thyroid gland is found in the neck, below the thyroid cartilage (which forms the laryngeal prominence, or "Adam's apple").
The thyroid gland controls how quickly the body uses energy, makes proteins, and controls how sensitive the body is to other hormones. It participates in these processes by producing thyroid hormones, the principal ones being triiodothyronine (T3) and thyroxine (sometimes referred to as tetraiodothyronine (T4)).
These hormones regulate the growth and rate of function of many other systems in the body. T3 and T4 are synthesized from iodine and tyrosine. The thyroid also produces calcitonin, which plays a role in calcium homeostasis.
Hormonal output from the thyroid is regulated by thyroid-stimulating hormone (TSH) produced by the anterior pituitary, which itself is regulated by thyrotropin-releasing hormone (TRH) produced by the hypothalamus.
The thyroid, a butterfly-shaped gland in the neck, can have a dramatic
impact on a huge variety of bodily functions, and if you're a woman over
35 your odds of a thyroid disorder are high—more than 30%, by some estimates.
At least 30 million Americans have a thyroid disorder and half—15 million—are silent sufferers who are undiagnosed, according to The American Association of Clinical Endocrinologists. Women are as much as 10 times as likely as men to have a thyroid problem, says integrative medicine specialist Robin Miller, MD, co-author of The Smart Woman’s Guide to MidLife & Beyond.
At least 30 million Americans have a thyroid disorder and half—15 million—are silent sufferers who are undiagnosed, according to The American Association of Clinical Endocrinologists. Women are as much as 10 times as likely as men to have a thyroid problem, says integrative medicine specialist Robin Miller, MD, co-author of The Smart Woman’s Guide to MidLife & Beyond.
The thyroid gland is covered by a thin fibrous sheath, the capsula glandulae thyreoideae, composed of an internal and external layer.
The external layer is anteriorly continuous with the pretracheal fascia and posteriorolaterally continuous with the carotid sheath. The gland is covered anteriorly with infrahyoid muscles and laterally with the sternocleidomastoid muscle also known as sternomastoid muscle.
On the posterior side, the gland is fixed to the cricoid and tracheal cartilage and cricopharyngeus muscle by a thickening of the fascia to form the posterior suspensory ligament of thyroid gland also known as Berry's ligament.
The thyroid gland's firm attachment to the underlying trachea is the reason behind its movement with swallowing.
In variable extent, the pyramidal lobe is present at the most anterior side of the lobe. In this region, the recurrent laryngeal nerve and the inferior thyroid artery pass next to or in the ligament and tubercle.
Between the two layers of the capsule and on the posterior side of the lobes, there are on each side two parathyroid glands.
The thyroid isthmus is variable in presence and size, can change shape and size, and can encompass the pyramidal lobe (lobus or processus pyramidalis.
The thyroid is one of the larger endocrine glands, weighing 2-3 grams
in neonates and 18-60 grams in adults, and is increased in pregnancy.
In a healthy patient the gland is not visible yet can be palpated as a
soft mass. Examination of the thyroid gland is carried out by locating
the thyroid cartilage and passing the fingers up and down, examining for
abnormal masses and overall thyroid size.
Then, place one hand on each
of the trachea and gently displace the thyroid tissue to the
contralateral side of the neck for both sides while the other hand
manually palpates the displaced gland tissue; having the patient flex
the neck slightly to the side when being palpated may help in this
examination.
Next, the two lobes of the gland should be compared for
size and texture using visual inspection, as well as manual or bimanual
palpation. Finally, ask the patient to swallow to check for mobility of
the gland; many clinicians find that having the patient swallow water
helps this part of the examination.
In a healthy state, the gland is
mobile when swallowing occurs due its fascial encasement. Thus when the
patient swallows, the gland moves superiorly, as does the whole larynx.
The thyroid is supplied with arterial blood from the superior thyroid artery, a branch of the external carotid artery, and the inferior thyroid artery, a branch of the thyrocervical trunk, and sometimes by the thyroid ima artery, branching directly from the subclavian artery.
The venous blood is drained via superior thyroid veins, draining in the internal jugular vein, and via inferior thyroid veins, draining via the plexus thyreoideus impar in the left brachiocephalic vein.
Lymphatic drainage passes frequently the lateral deep cervical lymph nodes and the pre- and parathracheal lymph nodes. The gland is supplied by parasympathetic nerve input from the superior laryngeal nerve and the recurrent laryngeal nerve.
In most cases, thyroid cancer presents as a painless mass in the neck.
It is very unusual for thyroid cancers to present with symptoms, unless
they have been neglected. One may be able to feel a hard nodule in the
neck. Diagnosis is made using a needle biopsy and various radiological
studies.
Other disorders
- Limited research shows that seasonal allergies may trigger episodes of hypo- or hyperthyroidism.
- Some rapid-cycling versions of bipolar disorder seem to have a complex relationship with thyroid dysfunction, however the specifics of the relationship are poorly understood.
Thyroid function tests
| Test | Abbreviation | Normal ranges[31] |
|---|---|---|
| Serum thyrotropin/thyroid-stimulating hormone | TSH | 0.5–6.0 μU/ml |
| Free thyroxine | FT4 | 7–18 ng/l = 0.7–1.8 ng/dl |
| Serum triiodothyronine | T3 | 0.8–1.8 μg/l = 80–180 ng/dl |
| Radioactive iodine-123 uptake | RAIU | 10–30% |
| Radioiodine scan (gamma camera) | N/A | N/A - thyroid contrasted images |
| Free thyroxine fraction | FT4F | 0.03–0.005% |
| Serum thyroxine | T4 | 46–120 μg/l = 4.6–12.0 μg/dl |
| Thyroid hormone binding ratio | THBR | 0.9–1.1 |
| Free thyroxine index | FT4I | 4–11 |
| Free triiodothyronine l | FT3 | 230–619 pg/d |
| Free T3 Index | FT3I | 80–180 |
| Thyroxine-binding globulin | TBG | 12–20 ug/dl T4 +1.8 μg |
| TRH stimulation test | Peak TSH | 9–30 μIU/ml at 20–30 min. |
| Serum thyroglobulin l | Tg | 0-30 ng/m |
| Thyroid microsomal antibody titer | TMAb | Varies with method |
| Thyroglobulin antibody titer | TgAb | Varies with method |
As of early 2014, in the United States, new guidelines for TSH levels have been implemented as endorsed by The American Association of Clinical Endocrinologists. the new range is a TSH of 0.3 to 3.0. Many testing facilities and doctors are still unaware of the change.
wikipedia.org



















0 comments:
Post a Comment